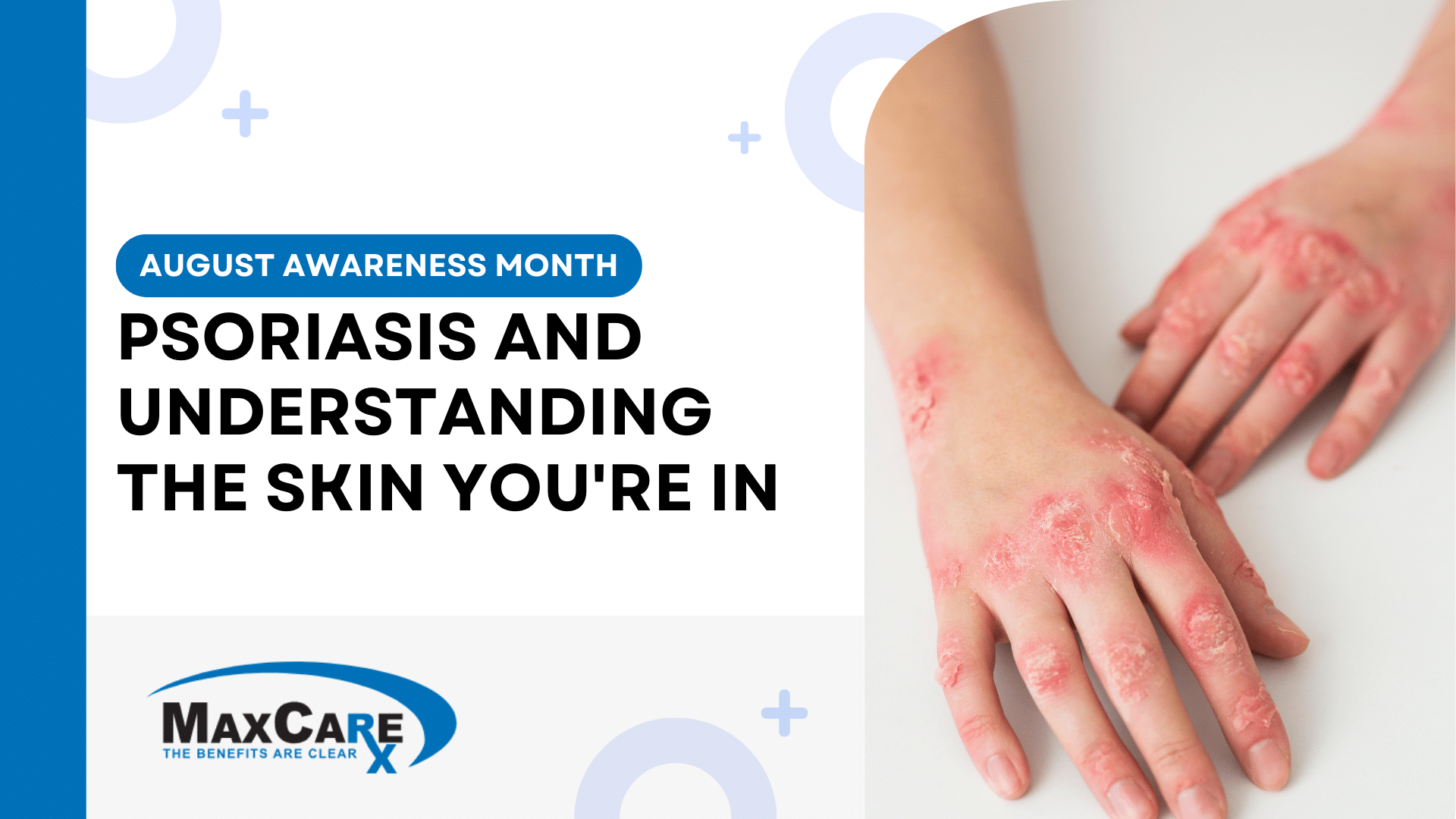
Psoriasis is a chronic, autoimmune skin disorder that accelerates the growth cycle of skin cells. This results in patches of thick, red skin covered with silvery scales. These patches, known as plaques, commonly appear on the elbows, knees, scalp, and lower back but can manifest anywhere on the body.
August is designated as Psoriasis Awareness Month, a time to shed light on a prevalent yet often misunderstood condition that affects millions worldwide. Let’s explore what psoriasis is, its prevalence, varying severity levels, and the importance of a layered approach in treatment to ensure optimal outcomes at minimal costs.
Who Psoriasis Can Affect
Psoriasis does not discriminate — it can affect individuals of any age, gender, or ethnicity. However, it typically manifests in two age peaks: between ages 20 and 30, and then again between ages 50 and 60. While both men and women are equally prone to the disease, the severity can vary substantially from one individual to another.
Prevalence and Quality of Life
Psoriasis affects approximately 2-3% of the global population. For many, the condition impacts not just physical health but also emotional and psychological well-being. The stigma and discomfort of living with visible skin lesions can lead to social isolation, depression, and anxiety. Therefore, addressing psoriasis effectively is crucial for improving patients’ overall quality of life.
Severity Levels
Psoriasis severity ranges from mild to severe and can significantly influence the choice of treatment. Here’s a closer look:
- Mild Psoriasis: Affects less than 3% of the body. Patients typically deal with minor irritations and a few localized patches of red skin covered with silvery scales. Even though it’s classified as mild, it can still cause discomfort and emotional distress if the patches are in visible or sensitive areas.
- Moderate Psoriasis: Affects 3-10% of the body. Those with moderate psoriasis may experience more widespread scaling and inflammation. The plaques are often more numerous and may require a combination of treatments including topicals and phototherapy to manage symptoms effectively.
- Severe Psoriasis: Affects more than 10% of the body. Severe cases of psoriasis involve extensive plaques that can cover large areas, affecting daily activities and significantly impacting the quality of life. These individuals often require systemic treatments (oral, injectable, or intravenous medications) to mitigate symptoms and control flare-ups.
Differentiating Psoriasis from Other Skin Conditions
While psoriasis is often confused with other skin conditions like eczema, there are notable differences:
- Psoriasis: Characterized by thick, red plaques with silvery scales. It is an autoimmune disorder.
- Eczema: Often presents as itchy, red patches and is generally triggered by allergens or irritants rather than an autoimmune response.
Both conditions require different management strategies, and misdiagnosis can lead to ineffective treatment and prolonged patient distress.
Treatment Approaches for Psoriasis
Psoriasis treatment can be multi-faceted, ranging from topicals to systemic therapies, depending on the severity and individual patient response.
It’s important to tailor treatments to ensure efficacy while managing costs. Older, well-established medications can be very effective for many patients, but newer treatments, including biologics, can be significantly more expensive. Therefore, a layered approach using treatment algorithms can help ensure that the lowest-cost, equally effective medications are utilized first, reserving costlier options for cases where necessary.
While there is currently no cure for psoriasis, its symptoms can be effectively managed through appropriate and consistent treatment regimens. Treatments aim to control the disease’s activity, reduce inflammation, and alleviate the skin plaques:
- Topical Treatments: These are often the first line of defense, including corticosteroids, vitamin D analogs, and salicylic acid. They can reduce inflammation and slow down skin cell turnover.
- Phototherapy: Light therapy uses specific wavelengths of light to slow skin cell growth and reduce scaling and inflammation.
- Systemic Treatments: For more severe cases, systemic treatments are used and they include oral medications, injectables, and intravenous therapies. These treatments work throughout the body to calm the immune system’s overactivity. They range from conventional systemic agents to newer biologic drugs, which specifically target parts of the immune system.
Given the chronic nature of psoriasis, management often requires a diligent and sustained effort, tailored to the severity and individual response.
Misconceptions and Spread
Common Misconceptions:
One common misconception about psoriasis is that it is contagious; however, this is entirely unfounded. Psoriasis cannot be spread from person to person through direct contact, sharing personal items, or any other means of transmission. The confusion often stems from the visible and sometimes severe appearance of the plaques and scales, which can resemble infectious skin conditions. However, psoriasis is strictly an autoimmune disease, meaning that it is caused by an abnormal reaction of the immune system.
Understanding Autoimmune Nature:
Psoriasis occurs because the immune system mistakenly attacks healthy skin cells, triggering an accelerated skin cell production cycle. This results in the rapid buildup of cells on the skin’s surface, forming the characteristic plaques. Unlike infections, which are caused by external pathogens like bacteria or viruses, autoimmune diseases arise from intrinsic issues within the body’s immune system. This intrinsic nature fundamentally separates psoriasis from contagious diseases.
Misconceptions Regarding Triggers:
Another misconception involves the triggers of psoriasis flare-ups. Many believe that they can predict or avoid flare-ups entirely; however, triggers can vary widely among individuals and can include factors such as stress, infections, changes in weather, medications, and lifestyle choices like smoking and alcohol consumption. Understanding these triggers is crucial for effective management, yet it is equally important to recognize that they are not consistent or universal.
Psychosocial Impact and Stigma:
The misconception that psoriasis is contagious contributes significantly to the psychosocial burden on patients. Many individuals with psoriasis face stigma, social isolation, and discrimination due to the visible nature of their condition. This can lead to considerable emotional distress, including anxiety, depression, and a lowered quality of life. Educating both patients and the public about the non-contagious, autoimmune nature of psoriasis is essential for reducing stigma and improving social acceptance.
Triggers and Risk Factors
Psoriasis flare-ups can be triggered by several factors, including:
- Stress: Physical and emotional stress can provoke flare-ups.
- Infections: Certain infections, such as strep throat, can trigger onset or flare-ups.
- Weather: Cold, dry weather can worsen symptoms.
- Medications: Certain drugs can exacerbate psoriasis symptoms.
- Lifestyle Factors: Smoking and heavy alcohol consumption are known risk factors.
MaxCare’s Approach
Understanding psoriasis, its treatment strategies, and the importance of a layered approach can lead to more effective management and better patient outcomes. As we honor Psoriasis Awareness Month this August, let’s commit to educating ourselves and advocating for cost-effective, efficient treatment protocols that benefit both patient and provider.
At MaxCare, we prioritize a layered approach, ensuring the right medication reaches the right member to achieve the best possible outcomes at the lowest possible costs. By leveraging treatment algorithms and cost-effective strategies, we help manage healthcare expenditures while maintaining high standards of patient care. Our goal is to provide tailored solutions that address the unique needs of each individual, ensuring effective and affordable treatment options for managing psoriasis.